by Craig Klugman, Ph.D.
Like most members of the American Society for Bioethics & Humanities (ASBH), I received an email last week geared toward enticing me to sign up to take the new Healthcare Ethics Consultant accreditation exam. The email offered a teaser question (one that really made no sense) and a link to view 15 sample questions to encourage me to pay $450 to take a test and get a Good Ethicist seal of approval. After going through these sample questions and seeing the answers (I got 13 out of 15 “correct”), I can say that with this new exam, my greatest and wildest fears for our field have come true.
At the beginning of July, I wrote about my concerns that the credentialing process might fracture “bioethics” into a number of subfields. I expressed my worry that the usefulness of clinical ethics would be lost when it is standardized and there is one way of thinking about cases. In one section, I wondered how the test writers would determine the “right” way to approach cases since there are so many competing methods taught in various schools.
As it turns out, the reason I got one question wrong was because I was not trained at the one institution that teaches that specific method. The question asked “Which of the following is an effective mediation strategy that can enable surrogate decision-making that meets ethical standards?” You are then offered four possible answers in a multiple choice format: Two of the possible responses were about “STADA” and two were about “CECP”. Clearly, this was a question asking if I knew what the acronyms were. Now I have been working and studying In the field of bioethics for 20 years. I’ve been involved with clinical ethics services at 6 different hospitals in different parts of the country. I have learned about CASES and ACES, facilitation and mediation. Most of these are borrowed from other disciplines or are shorthands created by education programs as tools for teaching their students a process.
I had never heard of either of these acronyms. The first possible response for STADA suggests it might stand for “Sit down, tell me about Mama, admire, discuss, ask.” I figured that could not be the answer because it’s incredibly sexist, ageist, and talks down to the patient. Two of the options privileged the clinical perspective (note, a response that does this is always wrong in examworld). The remaining response is “CECP: Clinical ethics conversation process.” I never heard that acronym before but it makes more sense than assuming every patient is an older woman who had children. Turns out that my reasoning was wrong: Mama was the correct answer. How can that be I thought?
I conducted a PubMed and Google search and found a few references to STADA in the literature, but always when talking about one institution’s (and only one’s) approach to a moderated mediation method. In an independent health news website, FierceHealthcare, there is an interview with a well-known ethics figure from a New York City area school where she describes STADA as written about in her book. In talking about this question with a colleague, she told me that the acronym CECP also comes out of this same program. Another colleague wth whom I spoke was also concerned because his training was that there were multiple ways to approach a consult (he works as a consultant).
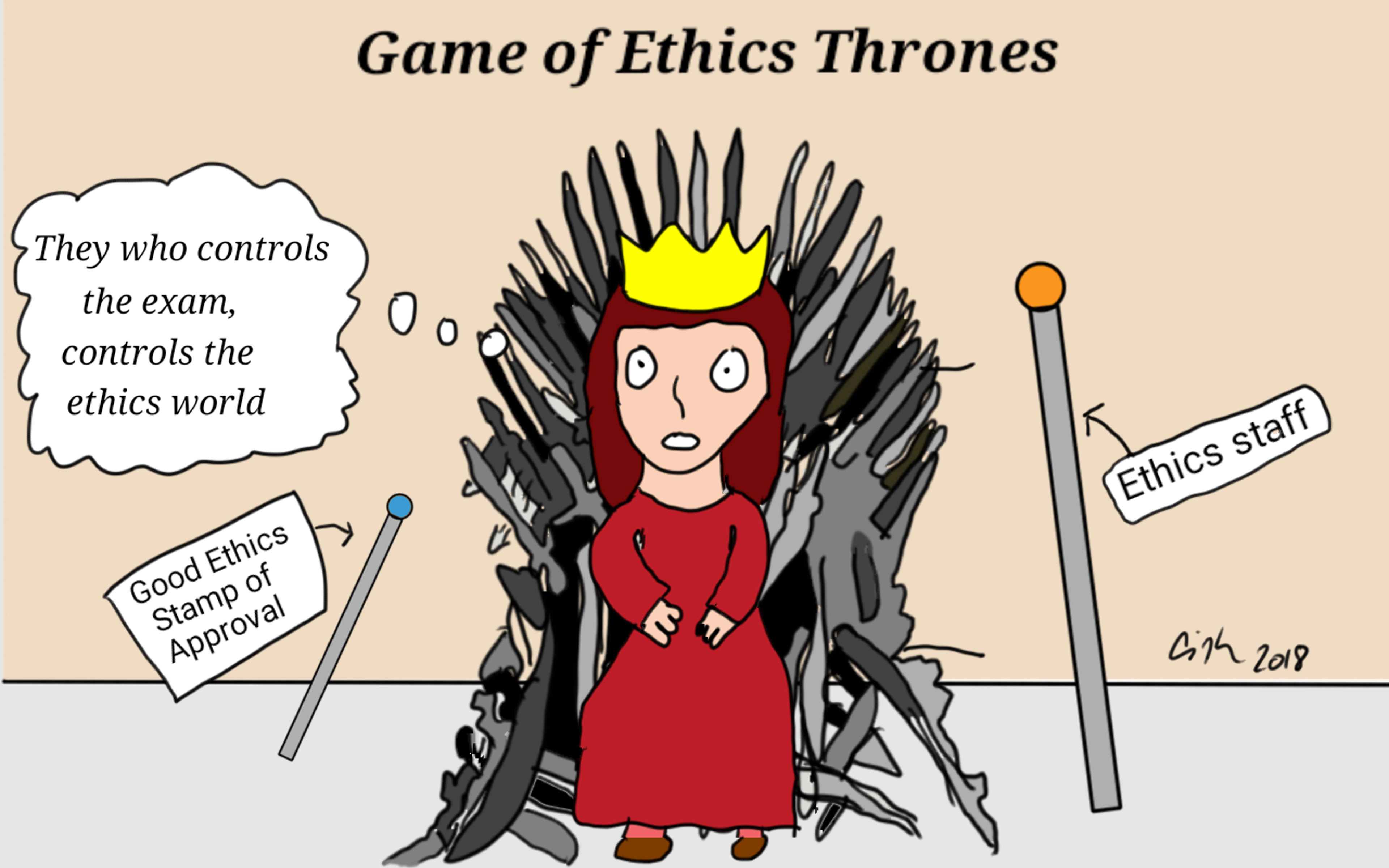
As political linguist George Lakoff taught the world, whoever defines the language has already won the debate. I realized that the examination is not about making sure that people who claim to be clinical ethicists can ably represent the field as the ASBH website states, but rather it is about which “school of thought” and which singular way of doing clinical ethics (i.e. you have to take their training program and read their books) is the “right” one. This exam, as it is being released, is all about who will control the future of clinical ethics consultation (excuse me, CECP).
My second concern with the sample questions follows on the first, the test assumes that there is a single, “right” way to do clinical ethics consultations. Several questions ask what step you would take first or what is the best response and then lists several possible answers. The problem is that depending on your institution, your experience, and your training, you might conduct the “steps” of a consult in different orders, or you might return to certain steps more than once, or you might do two simultaneously. In other words, many questions had more than one appropriate answer, but the test writer had one “right” way of doing it in mind. For example, one question asked about a transplant consult and which topic would be inappropriate to be raised with an attending physician. The possible answers include perceptions of the value of clinical ethics at the institution, questioning clinical judgement, concerns about institutional statistics, and a sense of responsibility. As a non-clinician, I would never question a clinical judgement without first talking with clinical providers who offer other perspectives and reasons, but apparently that was acceptable. The correct answer was that I should not share any criticisms of ethics services. Really? Self-preservation in the bureaucracy is the correct answer?
Third, the questions all assume that each person practices as a solo clinical ethics consultant. One question asked you to delineate the legal difference between surrogate decision-making and substituted judgement. The ideas are similar but there are technical differences in meaning. My concern from the scenario was the overarching question about making decisions for the patient. If I need to know a terminology distinction, I would look it up or speak with a legal member of the consult team. But being a member of a consult team is not an option on this exam. (Yes, this was the second question I got wrong).
Fourth, although it’s easiest to grade, does anyone think multiple choice for an ethics exam is a good idea? When I was at UT-Health San Antonio and we moved to a new integrated curriculum, I had to write ethics exams that followed the USMLE model of question writing. I was given training in how to do this and every question was reviewed by a committee. Every time my questions were reviewed, the committee exclaimed how difficult it was to write these questions because nuance was so important and there was so much grey area. In my 20 years of teaching, most every bioethics teacher I have spoken to on the undergraduate medical and baccalaureate level has said that multiple choice questions make little sense in bioethics. As I teach my students: It’s rarely about right and wrong or even the grey space, it’s about exploring all the colors of the rainbow. The better way to test ethics skills and knowledge is through conversation and essays—giving students an opportunity to explain their reasoning. Most falls, at Northwestern Feinberg School of Medicine, I help administer oral exams to the MS students. Students are given a case scenario which they individually present to two faculty members: Explain what the issues are, what ethical theories they would apply, and what conclusions they reach. In my bioethics course, the term finishes with oral debates where students demonstrate their critical thinking, research, listening, reasoning and argumentation skills. They also write a 10-page position paper where they argue pro or con on a controversial issue. That’s a better way to grade bioethics skills. The problem, of course, is that grading all of those papers takes a lot of time. And in teaching the medical school class, who has the time to grade essay exams of 220 students? In this particular case, though, we are not talking about whether medical students know to call for a consult or can recite the Four Principles. We are talking about an exam that determines who can practice as a clinical ethicist and that says there is a single right answer to how to the job—Hidden message: Ethics is about my right and everyone else’s wrong, not a process of moral deliberation.
What is one to conclude from this snapshot into the credentialing exam? One walkaway is clinical ethics is now about the right answer and the one true process, rather than a broader process of deliberating on complicated issues in complex situations. The second is that this exam is about power—who will be the arbiter of how one must do consults. When the “right” answer is an esoteric method created and taught in only one program in the country, it is saying that only people who have come out of that program are qualified to do consults. This is nothing less than a powerplay for the heart and soul of clinical health care ethics.