by Daniel Du Pont, MD, MBE and Jill Baren, MD, MS, MBA, FACEP, FAAP
The novel coronavirus outbreak, like any pandemic, has brought with it many difficult choices. When demand for medical resources exceeds supply, healthcare providers have to make excruciating decisions about which patients will be offered treatment—not just intensive treatments, but any basic life support measures. The fundamental problem of rationing is that the distribution of hospital resources and services, such as ICU beds or ventilators, is a zero-sum game: If the healthcare system is overwhelmed, each patient who receives treatment represents one or more others who do not.
In March 2020, the University of Pennsylvania Health System was beginning to experience an increase in the number of patients with COVID-19 who were sick enough to require hospital admission and, in many cases, critical care. While most of these patients came from our normal catchment area, many came from a significant distance. For example, more than twenty patients traveled from a single town in eastern New Jersey, about 75 miles away. Many of them arrived via private ambulance, bypassing dozens of closer hospitals. Some of those patients were critically ill upon arrival, with more than one requiring immediate intubation.
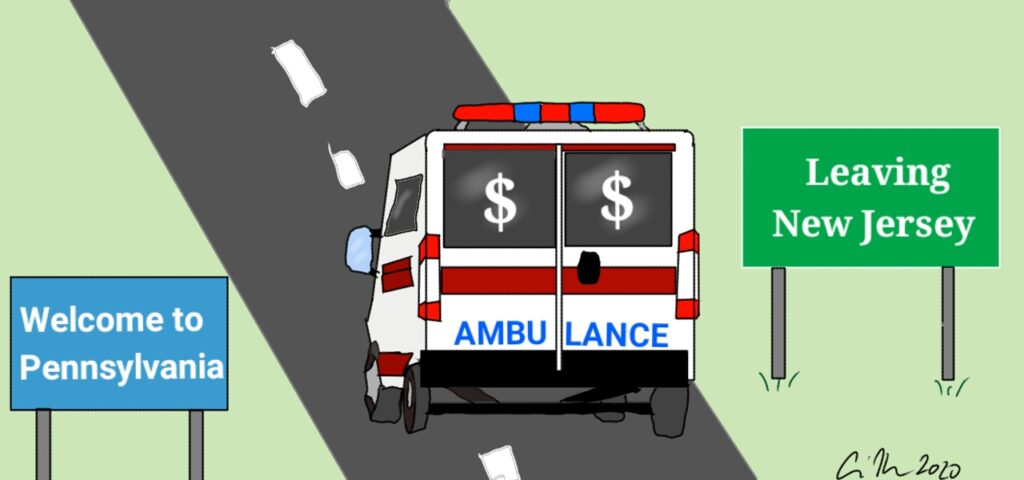
During this time, our hospital system had adequate resources to accommodate both patients in our typical catchment area as well as those beyond. However, when a cohort of patients uses personal means to travel significant distances in order to seek resources that have become scarce, it raises justice concerns. International guidelines for allocation of resources during a pandemic recognize that socioeconomic status should not be used to determine a patient’s course of treatment in a pandemic (WHO 2016). Private ambulance chartering allows for a de facto prioritization of the wealthy over the poor (for the purposes of this discussion, wealth will be used to refer not only to financial wealth but also to social capital such as membership in a group that allows access to resources that are not as available to the general public).
Most Americans do not have the resources to charter a private ambulance or redirect a 911 response to their destination of choice. When New York City and the surrounding metropolitan area hospitals were inundated with coronavirus patients, this resulted in inadequate hospital capacity. Some patients from this region of scarce resources were able to seek care in Philadelphia via chartered ambulance, but this opportunity was not uniformly available to those who were less well-off. Based on the authors’ consultation with multiple experienced EMS administrators, there can be wide variety in cost depending on the specific agency. For the above example, the price could reasonably be at least $2000-3000.
Ambulance chartering is not only unjust to poorer patients in the area that wealthy patients are leaving, but also has the potential to be unfair to less privileged patients at their destination. If ICU beds or ventilators were to become scarce in Philadelphia, patients in our own catchment area would then be competing with patients arriving by charter from outside the region. Those local patients who do not themselves have the means to travel from increased to decreased scarcity (to travel from Philadelphia to Baltimore, for example) are therefore seeking care from an effectively smaller resource pool. Based solely on their lesser socioeconomic capital, they will have more difficulty obtaining adequate care, especially in the case of rationing.
In the setting of a pandemic, the obvious choice for providing oversight to prevent unfair resource allocation is the federal government. Such a system has been used, for example, by the Italian government to attempt to optimize the use of resources in response to the novel coronavirus. The Italian government helped to oversee the distribution of goods like ventilators and also provided aid in the transfer of personnel and critically ill patients between regions. Strong federal leadership in these areas has so far been lacking in the United States.
Some state and local governments have provided clear guidance, but many have not. In the absence of direction from higher levels of authority, individual hospitals and health systems are left to determine how to treat patients in a just manner regardless of their socioeconomic status, insurance status, or ability to pay. Healthcare organizations should consider implementing protocols that minimize any advantage that affluent patients might have with respect to access to scarce resources. For example, a hospital or emergency department could develop a written policy to consider declining distant transfers if resources are limited enough that accepting such transfers carries a reasonable chance of unfairly privileging people of a higher socioeconomic status either at the time of transfer or, based on the best available projections, in the near future.
Hospitals should also consider including geography as a consideration in triage scoring systems that are used during times when the healthcare system is severely stressed. The Pennsylvania Crisis Standards of Care for Pandemic Guidelines, among others, suggest allocating critical care resources by calculating a priority score for each patient. Such a score would be based principally on medical prognosis, but could also include other considerations such as increasing priority points for groups such as frontline healthcare workers.The addition of “area of geographic origin for transfer patients” as even a minor factor in this scoring system could help offset any disparity resulting from long-distance chartering. Importantly, in the interest of fairness, most allocation proctols say that socioeconomic status in and of itself should not be part of the scoring system.
It is important to note that neither hospital guidelines nor ethical concerns about injustice supersede providers’ duty to evaluate and stabilize any patient who presents under the Emergency Medical Treatment and Labor Act (EMTALA).Also, patients’ desire to seek care beyond their region when a local healthcare system is overwhelmed should not be viewed as intrinsically unethical. If applied universally, however, the proposition that all patients should use their socioeconomic capital to the greatest extent in order to seek care for themselves or their family members leads to injustice. Individual patients are motivated to seek what they think is the best care for themselves or their families. They are unlikely to willingly forgo such treatment solely on the basis of a population-based ethical argument.
If we accept that individuals are understandably self-interested when it comes to pursuing and receiving medical care, then we cannot solely rely on their self-restraint to equitably distribute scarce healthcare resources. Ultimately, it must be up to government authorities and healthcare systems to do so. To ensure that poorer patients are not unjustly disadvantaged, triage protocols should account for long-distance ambulance charters. Additionally, state and local licensing bodies should sanction ambulance companies that engage in inappropriate transfers. In the meantime, patients will continue to seek the best care they can. As healthcare providers, it is our duty to use every resource we have to help every patient who presents to us.