by Ann Mongoven, Ph.D.
A federal judge in Texas declared all of the Affordable Care Act unconstitutional. The ACA remains the law of the land as the case moves to appeal. The ruling directly threatens popular ACA protections such as the ban on discrimination against pre-existing conditions, the allowance of children on parents’ policies until age 26, and a minimum acceptable benefits-package. Democratic lawmakers are in an uproar opposing the decision while Republicans remain largely silent. Striking mid-term election results on Medicaid expansion suggest party lines on health care are changing in ways that could enable new bi-partisan dialogue.
The Trump administration continuously repeats that 28 million Americans cannot afford health insurance due to Obamacare. It is true, and morally unacceptable, that 28 million Americans are uninsured. However, it is not due to the ACA. The largest factor in current rates of uninsurance, affecting at least five and half million people, is the ineligibility of undocumented immigrants for employer-sponsored insurance, ACA-market plans, Medicare, or Medicaid. The second largest factor, affecting at least 3 million Americans, is the failure of all states to enact Medicaid expansion. Other factors include people being unaware of their eligibility for insurance plans, or people deciding the out-of-pocket costs for plans available to them remain too high.
Lawmakers originally intended Medicaid expansion under the ACA to be obligatory, but a successful legal challenge made it optional for states. Medicaid, a federal-state partnership to insure low-income Americans, is the second-largest insurer in the United States (second only to Medicare, the federal insurance program for Americans over 65). Medicaid now covers nearly 75 million people (23 percent of the US population), while one in three Americans are low-income. Expansion provides affordable insurance to those low-income Americans who lack employer-coverage but whose income surpasses levels that qualify either for traditional Medicaid or for federal subsidies to buy private insurance.
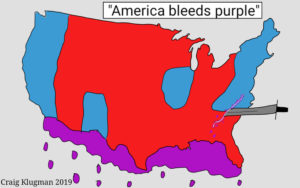
While commentators have lamented increasing polarization of voters into red and blue corners of the public square, election results on Medicaid expansion revealed universal concerns about health care access that transcend party lines. Ballot initiatives endorsing Medicaid expansion were passed in three Republican-led states (Idaho, Nebraska, and Utah) and rejected in one (Montana). Three additional states elected Democratic governors committed to Medicaid expansion (Maine, Kansas, Wisconsin). The Republican winner in Georgia’s razor-close gubernatorial election opposes expansion, despite a state survey suggesting a majority of Georgians in both parties favor it. Thirty-three states and the District of Columbia have enacted Medicaid expansion, with six more expected due to mid-term results.
Republicans had no alternative to the Affordable Care Act when they pulled back from their years-long threat to repeal it, a threat now judicially rekindled. Many Republicans, like all Americans, have pre-existing conditions or twenty-something kids. Democrats often insisted that health care is a right without discussing detailed policy visions. But many Democrats, like most Americans, struggle to pay increasing premium and other out-of-pocket-costs, and to negotiate complex systems of care. In the past, business and public-health sectors argued about where to locate the problem of the un- or under-insured. But new data proves that states which most successfully expanded insurance-access improved both public health andeconomic development. Not surprisingly, Americans of all political stripes yearn for a more dependable healthcare system.
Significantly, American civic discourse on health care has not always been characterized by predictable party polarization, and party-positions have flipped over time.
The development of employer-sponsored health insurance was an unintended consequence of wage and price controls during World War II. In the context of a wartime labor shortage, employers offered health insurance as a way around compensation caps. The perk was not conceived as a comprehensive healthcare system, and never functioned as one.
Some of the elemental bones of the ACA were first proposed by Republican President Richard Nixon in the late 1960s and early 1970s, against which Democratic Senator Ted Kennedy advocated a single-payer system. Nixon, whose childhood family had been financially devastated by healthcare costs, was determined to move the country toward universal coverage. Nixon and Kennedy came very close to offering a jointly sponsored compromise bill before the Watergate scandal closed the window of opportunity. Adaptations of Nixon’s plan were later advocated by several Republican governors before the successful 2006 adoption of (Republican) Governor Mitt Romney’s plan in Massachusetts, the prototype for President Obama’s ACA. At the time of its Democratic-passage in 2010, the ACA marked a Democratic political compromise to adopt what had long been the Republican-proposed strategy, viewed as the most consensus-generating path forward.
The ACA option to expand Medicaid initially was embraced by many Republican as well as Democratic governors seeking greater access for constituents. Despite subsequent pressure from the National Republican Committee, which adopted opposition to the ACA as a priority goal, by 2018 more than half of states with Medicaid expansion were led by Republican governors. However, not only disparities between expanded and unexpanded states, but also roll-backs of benefits in some expanded states during electoral shifts, have led to doubts about the adequacy of Medicaid expansion as a strategy for inclusive access.
The result is an extraordinary political moment: a moment when both many Democrats and many Republicans are actively supporting Medicaid expansion at the state level, and when both many Democrats and many Republicans are wondering whether more comprehensive health reform is needed. According to a recent national poll, a majority in both parties now favor exploring a single-payer system. An emerging consensus poses affordable insurance access as simultaneously a matter of justice, public health, support for families, and economic prosperity.
It should not be shocking to find party lines blurred as the nation struggles to address access to healthcare. Universal human mortality transcends all other political differences. Historical context reveals that there never has been a clear “Republican” or “Democratic” strategy to address challenges of healthcare access, quality, and cost. What is clear is the extent of those challenges. Also clear is America’s failure to meet them compared to other OECD countries—all of whose diverse healthcare systems score higher on access, cost-effectiveness, and quality.
Both our common mortality and the historical kaleidoscope of healthcare politics should free Americans to roll up our sleeves and work together to improve American healthcare. Americans of all party affiliation should:
- Endorse a moral commitment to catch up with other OECD nations on healthcare access, cost-effectiveness, and quality.
- Learn about the history of efforts to provide accessible health care in the United States.
- Learn what other OECD countries do to provide universal insurance enabling access to high-quality medical care. (Preview: they do different things.)
- Use precise vocabulary to talk about options. (For example, “Obamacare,” “a single-payer system,” and “socialized medicine” are not at all the same thing.)
- Put pragmatics ahead of ideology. We need a system that works more than we need a “red” or a “blue” system.
America bleeds purple. Perhaps in our common vulnerability, we will re-discover common purpose.