by Craig Klugman, Ph.D.
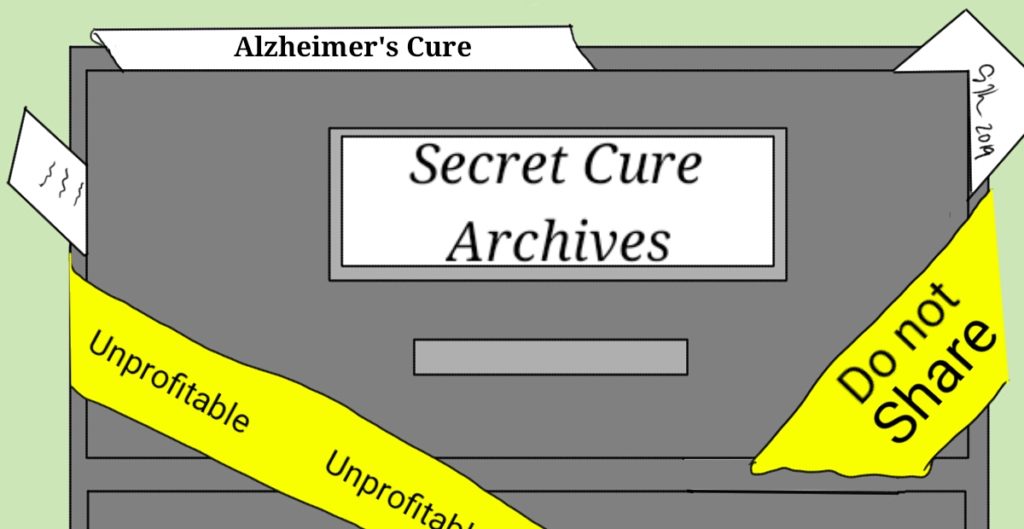
In 1983, NBC broadcast an alien invasion limited series calledV. In one episode, as the U.S. devolves into a tyranny, the military invades scientific labs and finds—inside the filing cabinets (it was pre-computer days)—cures for cancer and other diseases that were simply never released because companies made more money treating disease than curing it. From that 36 year old television image has come a modern reality—Pfizer may have a drug that improves the chances of preventing Alzheimer’s Disease, but they won’t pay for the clinical testing.
Enbrel is a $5 billion per year prescribed biologic medication approved in 1998 for rheumatoid arthritis. It has since been FDA approved for plaque psoriasis, ankylosing spondylitis, and polyarticular juvenile idiopathic arthritis. A recent Washington Post article reports that as of 2015, a Pfizer review of insurance claims found that the drug might also be effective in preventing Alzheimer’s, the 6thleading cause of death in seniors. Pursuing clinical trials for FDA approval would have cost $80 million, a direction the company did not pursue as Enbrel nears the end of its 20 year patent life (though an unrelated lawsuit is seeking to extend that period until 2029). However,The Postreports that Pfizer also chose to keep the data secret and not publish it, a step that would have allowed another company or group to perform trials. Interestingly, in 2018, Pfizer announced that it would no longer be working on treatments for Alzheimer’s.
This case raises a number of scientific and ethical questions:
(1) SCIENCE: Is Enbrel a treatment that can delay the onset or slow the progression of Alzheimer’s? No one knows though there is an intriguing possibility that it may. Stats 101 refresher: A correlation that people on Enbrel have lower rates of Alzheimer’s diagnosis is not proof of causation. A clinical trial would need to be done to answer this question.
(2) ETHICS: If there is a strong suggestion that a given drug has an effect on a disease, does the manufacturer have an obligation to pursue trials to test that hypothesis? Can a drug company abandon an area of inquiry because of reduced profitability or does it owe an obligation to society to find a potentially useful (and lucrative if its patent wasn’t ending) drug? Can companies be compelled to perform clinical trials that are promising if the company did not choose to pursue FDA approval for that prescribing purpose? The decision to pursue FDA approval is usually a business decision and in a [modified] capitalist society, companies and their boards have the freedom to choose what products to develop. Unless there is a declared emergency and public money made available for a company to produce or study a drug or a cure for a disease, there seems no way to for society to compel a company to act in any particular way (though a vote from the shareholders or a drop in share value can certainly influence decisions). From a business perspective, Pfizer’s decision makes sense. Why spend $80 million to prove that something works on a drug coming off patent. If the drug proves successful, then a generic manufacturer will reap the benefit of new sales, not the brand name.
However, a smart business decision is not necessarily a smart decision for the society or the public. In this case, there may be a duty (utilitarian; communitarian) for someone to pursue this line of research but it is not clear whose duty it would be.
(3) ETHICS: If the company chooses not to pursue the trial, is there an obligation to pass that information on to another company, the federal government, or a university to take on the research? This question is akin to the doctor who refuses to perform an abortion or prescribe birth control pills. At least before the establishment of the DHHS Conscience and Religious Freedom Division, a physician (or any health care provider) who would not perform a procedure or write a scrip had an ethical obligation to refer the patient to someone who would. With the new Division, there is no longer a legal obligation to do so, but the ethical obligation remains. Similarly, companies have no legal obligation to give away their trade secrets or to pass this information on to another company. Ethically, however, they do. Companies are enriched by the public buying their product and that creates a reciprocal obligation to provide a benefit for the public (to share the riches). The public relations benefits of working with other companies or university researchers to set up this trial would also provide a huge PR boon to the company, even if there was a hit to the next quarter’s bottom line.
(4) ETHICS and SCIENCE: Can double-blind placebo control trials ethically be done in this case when there is an agent that has shown a correlative connection to preventing (or slowing down) a disease, knowing that at least one arm of the study would not be getting the drug? One must consider that under the Declaration of Helsinki (to which the U.S. is not a signatory), a placebo controlled trial is not ethical if an arm of the study is receiving anything less than the current gold standard of treatment. At the moment, there is no medication that can prevent or slow down Alzheimer’s, though there are medications to help alleviate some symptoms. Most recommendations for prevention revolve around exercise, eating nutritiously and (sometimes) avoiding aluminum in the diet. Thus, it is possible that Helsinki would permit a placebo trial. Imagine this trial thought: Most subjects are likely to be people with a family history of Alzheimer’s and perhaps are even people who have the gene for the disease. Half of the participants would receive Enbrel and half would not. Given that there is a correlation between Enbrel and the onset of Alzheimer’s who would choose to be in the placebo group especially when they can simply ask their doctor for an off label prescription? This is not a case with zero evidence; there is correlative evidence.
(5) ETHICS: Can we ethically not do this study? Knowing there is an intriguing correlation, it seems that there may be an ethical directive to look deeper at this suggestion. The first step would be a larger epidemiologic study of existing insurance databases to see if the correlation holds with a larger set of records. If it does, then there would seem to be an imperative to see if correlation is causation. Given that there may be 13.8 million people with Alzheimer’s by 2050, is there not a need to see if any of these cases can be slowed, delayed, or prevented? If the answer is yes (and I think the answer is yes), then the question is, to whom does this imperative fall and who will pay for it? For that, I have no answers. Perhaps a patent extension on the drug could be dependent on completing clinical trials. Or perhaps a federal grant can be given to university researchers to complete this work.
(6) ETHICS: Did Pfizer commit and ethical faux pas when they hid these results rather than share this information? The answer is yes. While they may not have broken any laws, they certainly violated an ethics of transparency, responsibility, and working toward the better health of all. For this action, the company is ethically liable (might this require appearing before an ethics court?) and it would be intriguing if a case was brought to see if they were legally liable as well.
This is not the first situation where a company made an economic decision not to pursue a clinical trial. Physicians always have the right to prescribe a drug off label, but such efforts will not answer the question of whether this approach is actually effective. Then again, maybe that’s the intent, to leak this suggestion in order to increase long-term sales to the 13.8 million future Alzheimer’s patients. As strange as it may sound, that is the most likely of all these scenarios.