by Craig Klugman,PhD, Angira Patel MD, MPH, Nanette Elster, JD, MPH, and Dalia Feltman, MD, MA
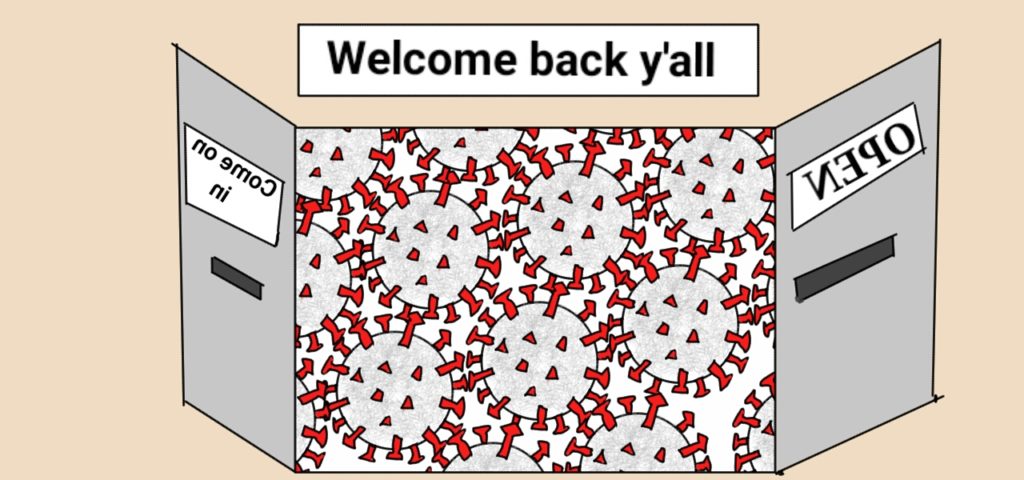
The debate continues on when and how to open the country back up and allow communities to return to “normal”. Consensus is lacking and there is significant variability across the country. The federal government rejected a CDC guideline for opening. Some states have come out with their own plans, and some states are just opening all the way through both governor orders and court decisions.
In many places, we have flattened the curve. However, flattening the curve now means moving more cases of COVID to later. A better metaphor than a curve is a balloon. We eliminated a bulge in the balloon at one point, but that just means we moved the bulge to another place. Until there is a vaccine (or a way to reduce the amount of air in the balloon), there has to be another bulge (or wave) in the future. This is why there is now discussion of a second wave.
 The Trump Administration has released a three phase plan for restarting our communities which first requires a decrease in the number of new cases for 2 weeks, hospitals moving out of crisis mode, and “robust testing” for health care workers. The World Health Organization has released six conditions before fully reopening society: 1. Expand, train and deploy your public health force, 2. Implement a system to find every suspected case, 3. Ramp up testing capacity and availability, 4. Identify and adapt key facilities to treat and isolate patients, 5. Develop a clear plan to quarantine contacts, 6. Refocus the whole of government on suppression and containing COVID-19. The US has not met any of these on a national level.
The Trump Administration has released a three phase plan for restarting our communities which first requires a decrease in the number of new cases for 2 weeks, hospitals moving out of crisis mode, and “robust testing” for health care workers. The World Health Organization has released six conditions before fully reopening society: 1. Expand, train and deploy your public health force, 2. Implement a system to find every suspected case, 3. Ramp up testing capacity and availability, 4. Identify and adapt key facilities to treat and isolate patients, 5. Develop a clear plan to quarantine contacts, 6. Refocus the whole of government on suppression and containing COVID-19. The US has not met any of these on a national level.
Epidemiologists report that living in harmony with COVID-19 means 58-70% of a given population must be immune. There are different ways to get to this steady state: developing, testing, and producing a vaccine in large quantities is one but that is anticipated to take 1-2 years. Alternatively, the country can allow natural infections in just the right amount while not overwhelming the health care system; to be sure, this is not ideal and would also lead to many deaths. If scientists find some effective antiviral medications, then the death rate may be lower.
From teaching the history of pandemics and treating patients, we know that things in the near future are dire: 1. Pandemics likely have multiple peaks necessitating multiple periods of physical distancing; 2. Herd immunity is far away and requires a vaccine or unacceptable sacrifice; 3. Medication supplies are dwindling; 4. Widespread testing is not enough; 5. Having the disease may not confer long-term immunity; 6. Health care providers are among the hardest hit populations; 7. Having had the disease may result in long-term health impacts and 8. Business and retail will have to adapt to a new way operating during periods of isolation.
This is not our nation’s first experience with a prolonged lack of normalcy; the U.S. recovered from two world wars and from a 1918-1920 influenza pandemic that killed 675,000 Americans. What got us through those crises were trusting scientists, solidarity toward a common goal, compassion for one another, and patience that someday things will be better.
Already the rapid change of adaptation is impressive. Industries have transitioned to manufacturing medical supplies. Health care professionals are rapidly running clinical trials and sharing information. Schools are adapting to remote instruction. Video conferencing has made physical distancing more social. Wearing masks has become a fashion trend and we will never again wash our hands for less than 20 seconds.
While patients are unlikely to outnumber ventilators and ICU beds right now, hospitals could be overwhelmed if communities open too soon or all at once. We urge patience, trust, caution and compassion in the age of COVID-19. The road ahead is long and difficult but together we can persevere.