The following editorial can be found in the April 2023 issue of the American Journal of Bioethics.
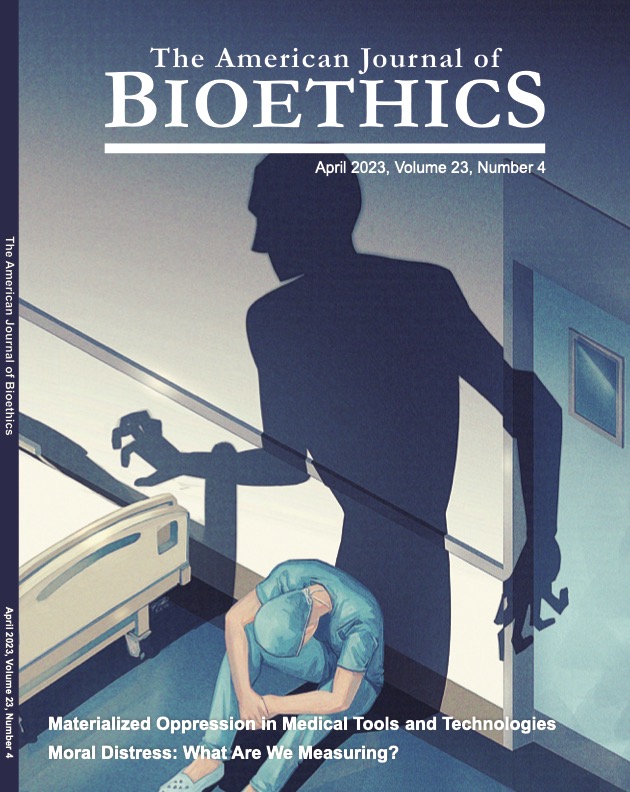
Liao and Carbonell’s article, “Materialized Oppression in Medical Tools and Technologies” directs our attention, not to new cutting edge medical technologies, but to the pulse oximeter and the spirometer, two devices that have been used in medical practice for decades. These devices have new relevance because they both measure aspects of respiration, and the ongoing COVID-19 pandemic is a disease that primarily affects the respiratory system. Like others, they state that both the pulse oximeter and the spirometer have failed to accurately capture aspects of respiration in Black people, Asian people, and others racialized as nonwhite, which has exacerbated the gross inequities in diagnosis, treatment, and outcomes of COVID-19 between white and nonwhite people in the US. Both devices have used white people as a norm, with the pulse oximeter using light skin as the norm and baseline to measure oxygen saturation, and the spirometer historically using white measures of lung function as the norm, and applying often invisible “corrections” to that norm for Black and Asian people. As the authors note, the history of “norming” to people racialized as white has been identified by historians like Lundy Braun, and as Boulicault (in this volume). These historical analyses show how concepts like the white “Reference Man” in medicine were used by white supremacists in the past like Samuel Cartwright, but continue to be used to reinforce these beliefs in the present. With the resurgence of public displays of white supremacist ideology through marches and murders, it is important for bioethicists to take note of the strong link between embedded white supremacy in medicine and the continuing embrace of this ideology outside of hospital walls. Actions like the Coalition to End Racism in Clinical Algorithms as Khazanchi et al describe (this volume) are important steps in this direction.
Although drawing attention to the harms of race norming in these two devices in the context of a pandemic is important, Liao and Carbonell’s piece makes three contributions to the discipline of bioethics that have not been previously highlighted in the scholarship on race-norming in medicine. First, the focus on the material aspects of medical devices encourages bioethicists to focus upstream on how these devices are designed and built, rather than a more traditional approach of focusing on the downstream effects of biomedical technology. This focus on the material features of devices also brings to bioethics the concept of enactment, one used in philosophy of science and medicine and science and technology studies (STS). Second, enactment allows conceptual space for bioethicists to explore processes of racial formation, racism, and other-isms that matter for health. As Baker notes (in this volume) and others, have argued, examining race and racism has been underexplored in bioethics, and the concept of materialized oppression in medical devices provides a way to explore racism as a structural dimension in medical practice and biomedical research. Third, the aggregated solutions approach is helpful for bioethics as it explores how to deal with racism and other -isms within the discipline, not just in the topics the discipline covers. In other words, the aggregated solutions approach can be used reflexively by bioethics as an institution to examine traditions and practices and to help the discipline move forward with solutions.
Material Properties, Upstream Focus, and Enactment
Liao and Carbonell’s concept of materialized oppression invites us to pay attention to the physical qualities of devices and their role in making discrimination and oppression real. This is complementary to the social determinist view of technology, which privileges the social as directing technology’s impacts, gives little to no attention to how the features of technology shape how it is used, taken up, and affect society. Focusing on the materiality of technological objects catalyzes thinking about distinctive, material features that can help reveal non-obvious functions and implications of these technologies. In this case, this focus on the features of these devices prompts analysts to “look under the hood” as it were, to examine the data and algorithms that power these devices. In the case of the pulse oximeter, their focus on how the device actually functions shows that oxygen saturation in the body is measured using light reflection, that this measurement can be taken on different parts of the body, and that current devices were generally validated in predominantly white populations. These differences, such as on whom devices are validated and whether oxygen saturation is measured on the ear or on the fingertip, have significant consequences, specifically less accuracy if skin is more pigmented than the selected reference. In the case of the spirometer, looking “under the hood,” means looking at how lung function values are calculated and outputs are determined. This leads the authors to the practice of racial correction and the history and beliefs that led to racial coefficients being invisibly inscribed into these tools. These cases provide instructive examples for bioethicists interested in examining the ethical dimensions of a new medical technology.
Instead of just looking at the technology that is available, there could be an examination of previous or alternate versions of the technology, an interrogation of data and references used to build it, and analysis of the design choices that resulted in the device that was ultimately brought to market and/or used in clinical practice. This carries particular relevance in spirometry where current interpretation now relies on race-specific equations (i.e., separate equations for white and Black patients that were derived separately from white and Black populations) rather than explicit “correction factors” applied to a single equation derived for white patients. Even if less explicit in norming whiteness than “correction factors,” current race-specific equations, when viewed from an upstream approach, directly descend from “correction factors” and continue to embody oppressive assumptions about an essentialized biological differences of race. Further, as we have previously argued, considering the upstream choices that led to current spirometry equations reveals other areas of lung function measurement beyond spirometry (i.e., lung volumes, and the ability of lungs to exchange oxygen and carbon dioxide) that rely on equations validated in white individuals, yet that have received considerably less attention. This kind of upstream focus on the material qualities provides a method for bioethicists to examine the ethical contours of medical devices and technologies in the past, present, and future.
In addition, the authors argue that focusing on the inner-workings of medical devices can reveal how these tools can materialize, or enact oppression. This concept of enactment has been explored in the philosophy of science and STS, such as in Mol’s description of the ways that heart disease is enacted, or brought into reality. For example, atherosclerosis can be enacted in different ways (in the same person) depending how it is identified and treated as a disease of the heart and/or of the legs. In the philosophy of science and medicine, the concept of enactment helps show how practices shape realities, and questions the notion of one objective truth, since practices can enact what can seem to be the same phenomenon (such as a disease) in multiple ways. Medical devices enacting oppression shows how medical practices can shape realities as well, and in particular how medicine can be a source of discriminatory harm, even without interpersonal racism. This is instructive for bioethicists because instead of, or in addition to looking at “implications,” we can examine enactments of scientific and medical technologies. An implications approach looks for effects of a tool, whereas an enactment approach charts the practices that create multiple realities that can then have sets of effects. Following an enactments approach may lead to the identification of more effects than an implications approach, and may also shed light on practices that can help explain how people from different groups can have vastly different experiences in identical clinical settings.
Materialized Oppression and Race in Bioethics
This article also contributes to the bioethical study of race and racism. In 2020, soon after the racial reckoning in the US, bioethics scholars voiced concerns about the lack of attention paid to race and racism in bioethics scholarship. There were calls for “black bioethics,” for example. Liao and Carbonell’s article makes a contribution to the bioethical study of race by showing how racial hierarchies become encoded into medical devices and thus play a part in reproducing those hierarchies and their associated harms. The article shows how race is similar and different in the two devices. In both devices, “whiteness is the norm and nonwhiteness a deviation”. However, race also works differently in the two devices since the pulse oximeter “does not deliberately account for race,” whereas the spirometer “deliberately accounts for race”. In addition, they note that the spirometer “essentialized social differences into innate biological differences,” whereas differences in skin pigmentation as measured in the pulse oximeter are a biological reality.
The authors provide insight on both the epistemology and ontology of race via these medical devices. For epistemology, they show how knowledge about race, specifically histories of scientific racism, influence the design of medical tools and become embedded in these devices. The article also prompts questions on the ontology of race—or what kind of “thing” race is—is it a social construct or a biological reality? They argue that the spirometer makes race, which is a social thing, an essential biological property of persons by adding racial corrections. This, they note, comes from a legacy of scientific racism, as espoused by historical figures such as Samuel Cartwright. However, the Cartwright quote they cite explains that he advocated slavery as necessary to help Black people improve their “weak” lungs, which shows that even in his view, race is not a completely essential biological property, since there is some mutability in lung function in Black bodies. In other words, in his conception, this property of Blackness (poorer lung function) seems to be able to be changed—to an extent. The paradox within Cartwright’s words also points to another paradox the authors identify, specifically that despite there being no genetic evidence associating race and lung function, “adjustment practices” persist in medicine, a field that is supposedly built upon objective research and the scientific method. The authors could interrogate these paradoxes further to illuminate the ontology of race in pulmonology specifically and in medicine more broadly. This kind of interrogation could shed light on the compelling example they raise of ethnic correction in spirometry between Han Chinese and other ethnicities in China. How are differences being conceptualized in this case? What kind of category of difference is “Han-ness?” Is it social, essentialized biological, or biological with some mutability? Questions like these relate to deKanter et al.’s plea (this volume) for thinking deeply about which differences matter. Liao and Carbonell’s observation that oppressive medical devices “deliver a measurement without the need for constant recalibration or deliberative cognition”, also relates to the productivity of race and racial categorization in medicine. Racial categories also provide a cognitive shortcut that can be useful in society and in medical practice, where the cognitive demands are high. The creation and dissemination of knowledge about race, the building of racial categories, and the functions of race in health and medicine are important aspects that bioethicists can explore through a focus on materialized oppression in medical devices.
Aggregated Solutions Framework for Bioethics
Liao and Carbonell argue that the pulse oximeter and the spirometer materialize oppression and create a moral aggregation problem that should be addressed with aggregated solutions. We propose thinking about racism in bioethics as a moral aggregation problem as well, as individual and other actions within bioethics as an institution can “interact in a system to generate significant harms in the aggregate”. If we apply the aggregate solutions framework to racism in bioethics, we will ask, what are the relevant attitudes, practices, and artifacts within bioethics? Bioethicist and philosopher Yolonda Wilson argues that an “epistemology of ignorance” permeates bioethics, and it is possible to conjecture that this epistemology affects the attitudes and practices of bioethics. As Wilson notes:
The epistemology of ignorance has enabled our field to minimize through inattention the role that racism plays in who lives and who dies and in how well one lives or dies. It has enabled serious discussion about whether calls to be explicitly antiracist are the proper domain of bioethics even though it is known that racism negatively impacts health.
If we apply the aggregated solutions framework to racism in bioethics (as a discipline), then we may also interrogate whether racism in the institution has the qualities of invisibility, expediency, and structural factors that Liao and Carbonell describe. In terms of invisibility, we can point to Baker’s contribution (this volume) that race and racism are missing from the formulation of bioethical principles. We can think of this absence in the way that Liao and Carbonell describe invisible oppressive features of medical devices—the absence of race and/or racism in the foundational principles of bioethics “hide[s] in a world where oppressive patterns are ubiquitous and therefore unremarkable” This relates to the racially discriminatory patterns of publishing and to the “white normativity” in bioethics. We can also ask how racism relates to expediency in bioethics. Are there defaults that are “easier” or “more convenient?” Could we view the largely white leadership in the discipline through the lens of expediency, as in, it’s “easier” to invite people with whom one is connected to through professional and personal networks to serve on committees and editorial boards? Might these “easy” and “convenient” practices require less cognitive demand, just as Liao and Carbonell argue that oppressive devices do? In the aggregated solutions framework, we can also ask about the structural factors that matter when we are thinking about racism in bioethics. Liao and Carbonell highlight healthcare’s profit-seeking motives as an important factor in explaining why the cheaper, but less accurate pulse oximeter became the preferred device. It may be fruitful to also interrogate structural factors that matter and can facilitate and reinforce racism in bioethics. Many bioethicists work in medical schools and soft-money environments where they depend on winning grants themselves or partnering with other investigators who win research awards. How does this incentive arrangement structure the kind of bioethics research that gets funded and then gets published? There is evidence that research grants focusing on health disparities are unfairly given lower ratings by reviewers. Does the drive to win awards to secure professional positions discourage bioethicists from pursuing or partnering with others whose research focuses on race and racism?
Conclusion
Our technologies and their use is a result of our choices, which were made in a distinct historical, social, political, and economic contexts. Liao and Carbonell’s article provides an account of how institutional racism is produced in medicine via medical devices. This is a departure from thinking of racism in medicine as interpersonal, clinician bias, and highlights the important connection between white racial norming and historical and current oppression and marginalization in medicine. But the article has a deeper resonance for the discipline of bioethics, specifically because it offers an upstream approach of examining medical technologies, a concept of enactment for understanding their effects, ways to think about epistemologies and ontologies of race, and an aggregated solutions framework that can not only illuminate the structural limitations of the field, but point to a path forward with multiple, layered solutions.
Disclosure Statement
KF is a member of the institutional review board for the National Institutes of Health’s All of Us Research Program and a member of the Digital Health Ethics Advisory Board for Merck KGaA. JHB has no interests to disclose.
Funding
The author(s) reported there is no funding associated with the work featured in this article.